Surgical Techniques in Oral and Skin Malignancy Treatment
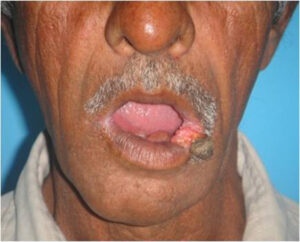
1. Carcinoma Lip - Estlander Flap:
Overview:
- Indication: Used for reconstruction after excision of carcinoma on the lower lip.
- Procedure: Involves the transposition of adjacent tissue to reconstruct the lip.
- Benefits: Preserves lip functions and aesthetics.
Step-by-Step:
- Step 1: Excision of the carcinoma with a safety margin.
- Step 2: Mobilization of adjacent tissue.
- Step 3: Transposition of tissue to reconstruct the lower lip.
- Step 4: Microvascular anastomosis for blood supply.
- Step 5: Closure of donor site.
Postoperative Care:
- Regular follow-ups to monitor healing and function.
- Speech and swallowing therapy if required.
- Scar management for optimal cosmetic results.
2. Carcinoma Tongue - Lateral Arm Flap:
Overview:
- Indication: Reconstruction post-carcinoma excision on the tongue.
- Procedure: Harvesting tissue from the lateral arm for reconstruction.
- Benefits: Provides reliable blood supply for tongue reconstruction.
Step-by-Step:
- Step 1: Excision of the carcinoma with adequate margins.
- Step 2: Harvesting tissue from the lateral arm.
- Step 3: Microvascular anastomosis for blood supply.
- Step 4: Shaping and suturing of the flap to reconstruct the tongue.
Postoperative Care:
- Intensive oral hygiene to prevent infections.
- Speech and swallowing therapy for functional recovery.
- Monitoring for signs of flap compromise.
3. Carcinoma Tongue - Radial Artery Forearm Flap:
Overview:
- Indication: Reconstruction for carcinoma on the tongue.
- Procedure: Utilizes tissue from the forearm, including radial artery for blood supply.
- Benefits: Offers a versatile flap with good vascular support.
Step-by-Step:
- Step 1: Carcinoma excision and identification of suitable forearm tissue.
- Step 2: Harvesting tissue including the radial artery.
- Step 3: Microvascular anastomosis for blood supply.
- Step 4: Shaping and suturing of the flap to reconstruct the tongue.
Postoperative Care:
- Strict monitoring for potential complications such as thrombosis.
- Physical therapy to maintain forearm function.
- Rehabilitation for speech and swallowing.


4. Mandible Reconstruction:
Overview:
- Indication: Carcinoma involving the mandible requiring extensive resection.
- Procedure: Microvascular free tissue transfer for bone, skin, and muscle reconstruction.
- Benefits: Restores facial aesthetics and preserves essential functions.
Step-by-Step:
- Step 1: Mandible resection with tumor removal.
- Step 2: Harvesting of tissue, often from the fibula, along with skin and muscle.
- Step 3: Microvascular anastomosis for blood supply.
- Step 4: Shaping and fixation of the transplant to reconstruct the mandible.
Postoperative Care:
- Intensive monitoring for flap viability.
- Rehabilitation for mastication and facial expressions.
- Long-term follow-up for function and aesthetics.

5. Nose Bilobed Flap:
Overview:
- Indication: Reconstruction following nasal carcinoma excision.
- Procedure: Utilizes a bilobed flap for rotation and reconstruction.
- Benefits: Addresses both cosmetic and functional aspects of nasal reconstruction.
Step-by-Step:
- Step 1: Excision of the nasal carcinoma with clear margins.
- Step 2: Design and elevation of the bilobed flap.
- Step 3: Rotation and suturing of the flap to reconstruct the nose.
- Step 4: Closure of donor site.
Postoperative Care:
- Nasal hygiene and care to prevent infection.
- Monitoring for flap viability and symmetry.
- Scar management for optimal cosmetic results.

Conclusion:
Advancements in surgical techniques for oral and skin malignancies have greatly improved patient outcomes, offering a combination of functional and aesthetic restoration. Close collaboration between surgeons, oncologists, and rehabilitation specialists ensures a comprehensive and effective approach to treating these complex cases. Regular follow-ups and postoperative care play a crucial role in achieving successful outcomes and enhancing the quality of life for individuals affected by oral and skin malignancies.
1. Q: What is the Estlander Flap, and when is it used?
- A: The Estlander Flap is a surgical technique used for reconstructing the lower lip after the excision of carcinoma. It helps restore both the form and function of the lip.
2. Q: What distinguishes the Lateral Arm Flap and Radial Artery Forearm Flap in tongue reconstruction?
- A: Both flaps are used for tongue reconstruction, with the Lateral Arm Flap utilizing tissue from the arm, while the Radial Artery Forearm Flap involves harvesting tissue from the forearm, including the radial artery for a reliable blood supply.
3. Q: When is Mandible Reconstruction necessary, and what does the procedure involve?
- A: Mandible Reconstruction is required when there's carcinoma involving the mandible, leading to extensive resection. The procedure involves microvascular free tissue transfer, including bone, skin, and muscle, to restore facial aesthetics and preserve essential functions.
4. Q: What is the purpose of the Bilobed Flap in nasal reconstruction?
- A: The Bilobed Flap is used to reconstruct the nose following excision of nasal carcinoma. It involves the rotation of two lobes of tissue to address both cosmetic and functional aspects of nasal reconstruction.
5. Q: How is blood supply maintained in these surgical procedures?
- A: Microvascular anastomosis is a common technique used in these procedures to establish a reliable blood supply for the transplanted tissue, ensuring its viability.
6. Q: What are the postoperative care considerations for these surgeries?
- A: Postoperative care involves regular follow-ups to monitor healing, speech and swallowing therapy if required, and scar management. Patients are closely monitored for potential complications, and rehabilitation is often essential for functional recovery.
7. Q: Can these surgical procedures be performed on elderly patients?
- A: The feasibility of these procedures in elderly patients depends on various factors, including overall health and the extent of the malignancy. Individual assessments by the surgical team are crucial to determine the appropriateness of these interventions.
8. Q: Are there alternative non-surgical treatments for oral and skin malignancies?
- A: Depending on the stage and type of malignancy, alternative treatments such as radiation therapy and chemotherapy may be considered. However, surgical interventions are often necessary, particularly in advanced cases.
9. Q: How long is the recovery period for these surgical procedures?
- A: Recovery periods vary based on the complexity of the surgery and the patient's overall health. Typically, initial healing occurs within weeks, but full recovery and rehabilitation may take several months.
10. Q: Are these procedures covered by insurance?
- A: Insurance coverage varies, and it's advisable to consult with both the surgical team and the insurance provider to understand the coverage for specific procedures, pre-operative evaluations, and postoperative care.